Prop 1
Gov. Gavin Newsom’s Proposition 1 is the latest milestone in California’s long struggle to address mental illness. It would allocate new funding for housing and treatment facilities, aiming to address a crisis that plays out on city streets.
BY JOCELYN WIENER, CalMatters
Fallout from our state’s long history of breaking promises to people with serious mental illness is everywhere.
It can be found under our overpasses and in our tent encampments, but also inside our jails and prisons, our emergency rooms, our schools, our homes.
It flashes across our public opinion polls, which repeatedly list mental health as a top concern.
Increasingly, it makes its way into our political discourse. Referencing “our broken system,” Gov. Gavin Newsom in recent years has rolled out mental health policies with dizzying speed.
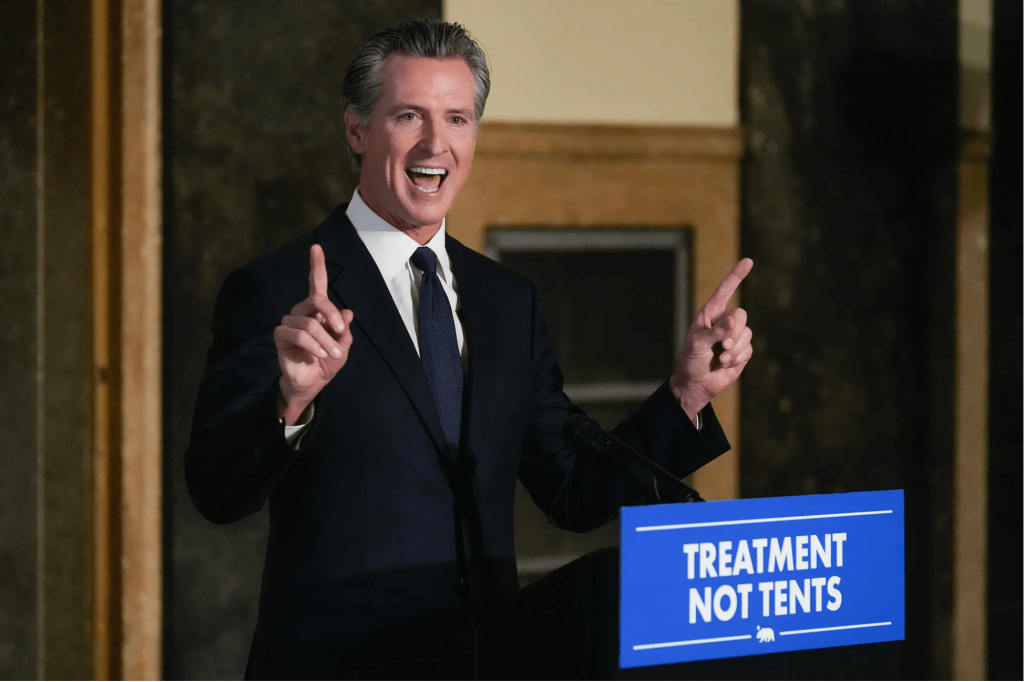
Now he’s promoting Proposition 1, a two-pronged March ballot measure that would fund a $6.4 billion bond for treatment beds and permanent supportive housing, while also requiring counties to spend more of their existing mental health funds on people who are chronically homeless.
The measure makes promises of its own.
“These reforms, and this new investment in behavioral health housing, will help California make good on promises made decades ago,” Newsom has said.
What are the promises that California has made to people with mental illness over the years? And why are so many people still suffering?
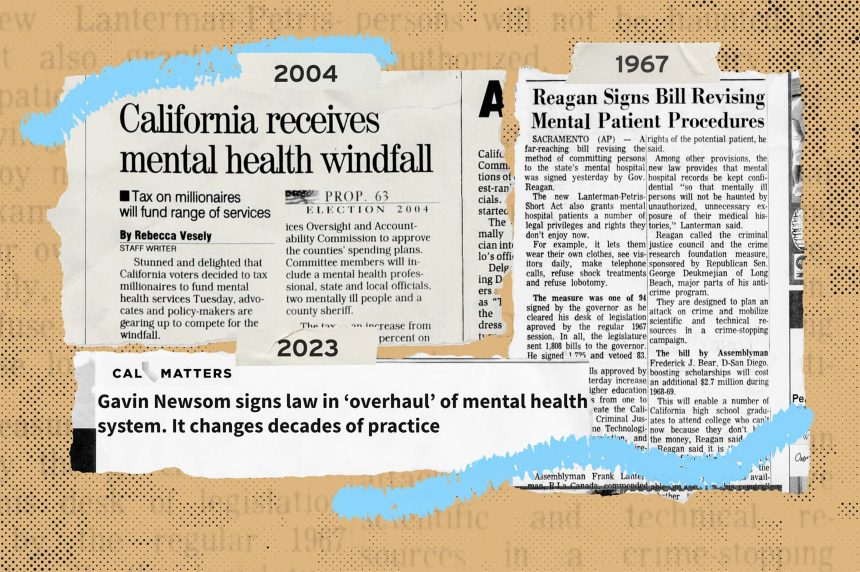
Here’s a brief timeline of mental health policies in our state—of promises made and promises broken—during the past 75 years.

1950s & 1960s:
An era of institutionalization
In the 1950s, it is relatively easy to force people into state mental hospitals, many of which have horrific conditions. The number of patients peaks in the late-1950s, at approximately 37,000. During that time, the state starts shifting control over mental health services to counties, embarking on the process of deinstitutionalization. This process accelerates in the late 1960s with the passage of the landmark Lanterman-Petris-Short Act, a law designed to protect the civil rights of people with mental illnesses.
1954:
The federal Food & Drug Administration approves Chlorpromazine (Thorazine), the first antipsychotic drug, to treat people with serious mental illnesses.
1957:
The California Legislature increases funding for community mental health under the Short-Doyle Act, aiming to treat more people in their communities instead of in state hospitals.
1963:
President John Fitzgerald Kennedy signs the Community Mental Health Act, promising federal leadership to build and staff a network of community mental health centers. Less than a month later, he is assassinated. Many of the clinics are never built.
1965:
Congress creates Medicare and Medicaid, allowing people with mental illnesses to receive treatment in their communities.
1967:
Then-Gov. Ronald Reagan signs the Lanterman-Petris-Short law limiting involuntary detention of all but the most gravely disabled people with mental illness and providing them with legal protections.
1970s & 1980s:
California tax revolt leads to austerity
As state mental hospitals close in the 1970s, many people with serious mental illnesses are moved into for-profit nursing homes and board and care homes. Their numbers on the streets and inside jails and prisons begin to rise. The 1980s sees significant funding cuts for mental health services at both the state and federal levels.
1978:
The Community Residential Treatment Systems Act seeks to create unlocked, noninstitutional alternatives for people with mental illness throughout California.
The same year, voters pass Proposition 13, capping property taxes and reducing the amount of money available to counties for a variety of services, including mental health.
1980:
President Jimmy Carter, who a few years earlier created a Presidential Commission on Mental Health at the urging of his wife Rosalynn, signs the Mental Health Systems Act to fund the community mental health centers envisioned by President Kennedy.
1981:
President Ronald Reagan signs the Omnibus Budget Reconciliation Act, repealing most of Carter’s Mental Health Systems Act and kicking responsibility for people with serious mental illness back to the states.
1990s:
Local control of mental health services
The decade sees funding and responsibility for mental health services shift from the state to counties. California passes a law to hold health plans accountable for providing adequate mental health treatment.
1991:
The state Legislature passes “realignment” — moving funding and responsibility for many mental health services from the state to counties.
1995:
The state implements Medi-Cal Mental Health Managed Care, making counties responsible for providing many Medicaid mental health services.
1999:
California passes a state parity law, requiring private health plans to provide equal coverage for serious mental illness and physical health.
The same year, the Homeless Mentally Ill Act — a pilot program to help homeless people with serious mental illness and an important precursor to the Mental Health Services Act — rolls out in three counties.
2000s:
New resources for mental health care
Optimism about the state’s ability to finally address the needs of people with mental illness surges with the passage of the landmark Mental Health Services Act. But the Great Recession in the later part of the decade threatens some of that progress.
2002:
The Legislature passes Laura’s Law. Named for a young woman killed by a man who refused psychiatric care, the law allows — but does not require — counties to build court-ordered treatment programs.
2004:
California voters approve the Mental Health Services Act. The 1% tax on people with incomes above $1 million provides a new source of revenue to bolster county mental health systems.
2008:
A federal parity law, the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act, requires health plans that offer coverage for mental health issues and substance use disorders to provide comparable benefits to those offered for medical and surgical treatments.
2010s:
Homelessness focuses attention
The numbers of people with serious mental illness experiencing homelessness continue to increase. Jails and prisons are now the country’s largest mental health providers, and a backlog of incarcerated people deemed incompetent to stand trial draws increasing scrutiny. The numbers of children and adolescents landing in hospitals in mental health crises begins to rise.
2010:
The Affordable Care Act (Obamacare) requires insurers to provide mental health as an essential benefit.
2011:
The Great Recession triggers significant budget cuts, pushing some people out of the public mental health system. A second movement or ‘realignment’ of mental health and substance use disorder services passes even more funding and responsibility from the state to the counties.
2012:
California eliminates its Department of Mental Health and distributes its responsibilities among other state departments.
2013:
The Mental Health Wellness Act injectsabout $143 million into increasing the capacity of the state’s mental health crisis response system.
2018:
California voters pass a ballot measure called No Place Like Home to build and rehabilitate supportive housing for people with mental illness. The measure authorizes the use of Mental Health Services Act funds to pay for $2 billion in bonds.
That same year, Newsom is elected governor and vows to make mental health a major focus of his administration.

2020s:
Newsom’s mental health agenda
In the wake of the COVID-19 pandemic, the sheer number of people with mental illness on the streets, along with the fentanyl epidemic and a growing mental health crisis among children and teenagers, leads to increased public interest in mental health. The Newsom administration makes unprecedented investments and rolls out a steady stream of major policy changes. Critics decry some of these changes as moving the state toward more involuntary treatment.
2020:
California passes a “groundbreaking” new state parity law, greatly expanding upon its earlier law and making it a national leader in requiring commercial health plans to provide mental health services.
2021:
The Newsom administration allocates $4.6 billion in one-time funds for a Children and Youth Behavioral Health Initiative.
2022:
The administration creates Community Assistance, Recovery, and Empowerment (CARE) Courts, new court systems to address the needs of people with serious mental illness that have some echoes of Laura’s Law. This time, county participation is not optional.
That same year, a massive statewide effort called California Advancing and Innovating Medi-Cal (CalAIM) begins rolling out, promising to expand and streamline access to mental health care for people insured by Medi-Cal, the public insurance program for low-income Californians.
2023:
Newsom signs a law that amends the definition of “grave disability” that was originally laid out in the landmark 1967 law limiting involuntary confinement in the state. The amendment makes it easier to conserve people with serious mental illness—stripping them of their rights and entrusting their care to public guardians.
2024:
Proposition 1 comes before the voters. If it passes, it will bring in billions of new funding for permanent supportive housing and treatment beds, and will place new parameters on how Mental Health Services Act funds are used.
This timeline was reported with the help of dozens of news articles and government and academic reports, as well as interviews and historical information provided by a variety of individuals, including Steve Fields, Adrienne Shilton, Michelle Cabrera, Corey Hashida, Stacie Hiramoto, Randall Hagar, Diane Van Maren, Chad Costello and Alex Barnard’s 2023 book “Conservatorship: Inside California’s System of Coercion and Care for Mental Illness”
For More California News Visit www.zapinin.com/california-news.