As California gears up for a winter of respiratory illnesses, health officials and providers often reference one encouraging factor — the greater availability of COVID-19 treatments and antivirals like Paxlovid. But many patients aren’t using them.
“We have a concerning low rate of outpatient COVID-19 treatments, especially for vulnerable populations,” Dr. Rohan Radhakrishna, chief equity officer at the California Department of Public Health, told doctors in an online event in November. “We want to remind the provider community that therapeutics are in ample supply and that most adults have qualifying conditions.”
Some county health officials agreed that more people should be taking advantage of these treatments. Patients may not be using them for a number of reasons, they said, including lack of awareness and confusion over who qualifies for a prescription. Add to that some people’s concerns over “Paxlovid rebound,” when people test positive again soon after having tested negative. There is also a need for easier and quicker access, experts say. Anecdotally, people have found some providers more strictly limit which patients get prescriptions.
Health officials say a key difference between this upcoming winter and the last two is the wider availability of COVID antivirals like Paxlovid. But many infected people aren’t aware of their availability or have difficulty accessing them.
The “misperception of drug scarcity” has resulted in some providers denying treatment to eligible people, the state’s public health department noted in a health notice sent to providers last week.
“I can share from personal experience from family members to my colleagues within the Department of Public Health who got COVID this summer — although they qualified for Paxlovid, it was really hard to get,” Radhakrishna said. People shouldn’t have to pull special strings to get these treatments, he said.
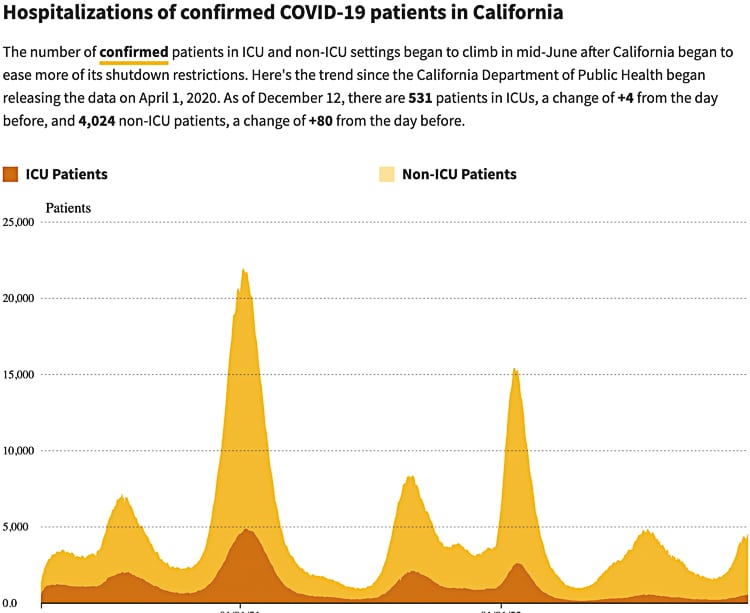
The department’s message comes as hospitalizations have more than doubled since Nov. 1, and the positivity rate is once again in the double digits — 10.8% as of the latest update on Thursday.
Paxlovid, the most commonly prescribed treatment, is an oral medication that can help reduce the severity and length of symptoms and decrease the chances of hospitalization. Pfizer, which makes the drug, reported in published clinical trials that it reduces the risk of severe COVID by 89%. Staying out of the emergency room is especially important when hospitals in parts of the state are being strained by other respiratory illnesses, health officials say. A second oral antiviral, Lagevrio, made by Merck, is also available with a prescription.
One year ago, the U.S. Food and Drug Administration approved the first antivirals for emergency use. The initial rollout was hindered by low supply and treatments were rationed during last winter’s omicron surge. Gradually, availability has increased, and the federal government and states have worked to increase the number of places where patients can get treatment.
As of Nov. 27, providers had administered 72% of all Paxlovid units allocated to California and 21% of Lagevrio, according to federal data. Nationally, those numbers were 66% for Paxlovid and 31% for Lagevrio.
The California Department of Public Health said in an email response that it did not expect the supply of antivirals to be an issue in case of another uptick in infections this winter.
National analyses of antiviral prescriptions have shown that despite the growing availability of these medications, uptake is lower in poorer zip codes — a disparity that was also seen with vaccination and testing. One possible factor: There tends to be fewer facilities with treatments available in rural and high-poverty counties, according to a national Kaiser Family Foundation analysis from this summer.
“A large part of it is just plain ignorance that they (treatments) are even out there.”
~ Dr. Rais Vohra, Fresno County’s Public Health OfficerDr. Rais Vohra, Fresno County’s public health officer, said one of the easiest ways to increase the use of antivirals is to promote them at the time of testing.
“At the time that you swab someone, we should say ‘I’m going to swab you. If it comes back positive, I want you to call this phone number and they can set you up with oral medications.’ That really should be the new model for COVID care for the outpatient setting,” Vohra said.
But that’s not the case in most places. And as more people test at home, the onus is on patients to learn on their own what’s available.
“A large part of it is just plain ignorance that they (treatments) are even out there,” Vohra said. “I think a lot of us are kind of anchored in the early days of the pandemic. However, now that these therapies have come along, we really need to change the mental model.”
Local health officials say there also needs to be greater clarity about who qualifies. Some people may be aware that antivirals are available, but they may not realize they themselves are eligible, so they don’t seek out treatment, said Dr. Jennifer Chevinsky, Riverside County’s public health officer.
For example, all people over age 50 should be screened for Paxlovid, Chevinsky said. And the state has asked local health departments and providers to look more broadly at the type of health conditions that can put people at high risk, she said.
Most adults actually have a qualifying condition, according to the state’s health department. These include a number of chronic diseases, hypertension, obesity, depression, smoking and physical inactivity.
One piece of advice from Chevinsky, especially for people who use other medications: They should contact their provider and make a plan even before they catch COVID. That way if people do become infected, they will already know whether they qualify for Paxlovid and how they can obtain it.
Experts say that while cases of Paxlovid rebound have received a lot of attention, that shouldn’t discourage people from taking it.
“People still have concerns about rebound and we want to remind people that the rate of rebound is low, less than 10%,” Radhakrishna said. “And rebound can occur anyway, even without Paxlovid treatment.” While research is ongoing, experts estimate the rebound rate is somewhere in the 2%-to-10% range.
How to access antivirals
The time frame to get a prescription also is tight — people need to start treatment within five to seven days from the onset of symptoms. Primary care providers may be the most convenient option because they already have a patient’s medical history on hand. For people who cannot reach their doctor within the five-day window or don’t have one, however, health officials recommend several other routes, including one-stop sites where people can both get tested and receive medication (also known as “Test to Treat” sites), and a recently launched statewide telehealth service.
Over the summer, the FDA changed its regulations to allow pharmacists to prescribe COVID pills. At large retail pharmacies, patients can seek a screening online and if deemed eligible, get their prescription delivered or picked up by a family member. While antivirals are free, at least one chain pharmacy, CVS, charges $60 for a consultation, according to its website.
People can also try the federal “Test to Treat” locator tool, which launched this past spring. This tool directs people to clinics, pharmacies and OptumServe sites. But there are still large swaths of the state, such as rural Northern California, that have few of these sites. For example, the closest “Test to Treat” location for someone living in Chico is in Red Bluff, about a 45 minute drive away, according to the map tool. There are, however, several local pharmacies there that can fill a prescription.
To bridge access gaps, the state also contracted with a telehealth service available to people statewide where they can schedule appointments. Virtual visits via Sesame Care are free to the patient and paid for by the state. According to the site, the service is available to people who are uninsured or having trouble seeing their primary care provider.
“The state is trying a lot of different models of “Test to Treat” and some of them are more successful than others,” Vohra said. “This Sesame platform is great because if you test positive, you can pick up the phone and talk to a prescriber over the phone. Not a lot of people are aware of it.”


Hello there! Do you know if they make any plugins to assist
with Search Engine Optimization? I’m trying to get
my blog to rank for some targeted keywords but I’m not
seeing very good success. If you know of any please share.
Many thanks! You can read similar article here: Bij nl
Thanks for sharing. I read many of your blog posts, cool, your blog is very good. https://www.binance.com/en-IN/register?ref=UM6SMJM3
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.
Your article helped me a lot, is there any more related content? Thanks! https://accounts.binance.com/en-IN/register?ref=UM6SMJM3
Hi! Do you know if they make any plugins to assist with SEO?
I’m trying to get my blog to rank for some targeted keywords but I’m not seeing
very good gains. If you know of any please share.
Thank you! You can read similar blog here: Change your life
Thanks for sharing. I read many of your blog posts, cool, your blog is very good.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
I’m extremely inspired together with your writing abilities as neatly as with the structure for your blog. Is this a paid theme or did you customize it yourself? Anyway stay up the excellent quality writing, it’s rare to see a nice weblog like this one these days. I like zapinin.com ! It’s my: Instagram Auto follow
I am extremely inspired along with your writing skills as smartly as with the format in your weblog. Is that this a paid subject matter or did you customize it your self? Either way keep up the nice high quality writing, it’s uncommon to see a great weblog like this one these days. I like zapinin.com ! My is: TikTok Algorithm